How a cyberattack disrupted the healthcare system and what can be done to prevent it in the future
UnitedHealth’s Change Healthcare recent cyber security incident highlights the growing vulnerability and attractiveness of the U.S. healthcare sector to sophisticated cybercriminals. This breach, occurring over three weeks ago, led to the U.S. Department of Health and Human Services launching an investigation due to its unprecedented scale. Change Healthcare, a key player in insurance billing and payments, has left countless healthcare providers unpaid since the February 21 attack as it struggles to restore its systems.
Interoperability and Single Points of Failure
The healthcare claims adjudication process in the United States is heavily reliant on a small number of large clearinghouses. These clearinghouses are pivotal in the healthcare financial ecosystem. They serve as crucial gateways for claim reimbursements and provide a range of essential services that underpin the delivery of healthcare. Their role is central to the operational efficiency of healthcare providers.
However, this concentration creates significant risks. The dependence on a few large clearinghouses has made the healthcare reimbursement system susceptible to major disruptions. The complexity of integrating billing systems across various payers and providers means that these clearinghouses are not just facilitators but also potential single points of failure. In some cases, payers mandate that claims be processed through a specific clearinghouse, forcing all associated providers to depend on a single entity for claim adjudication.
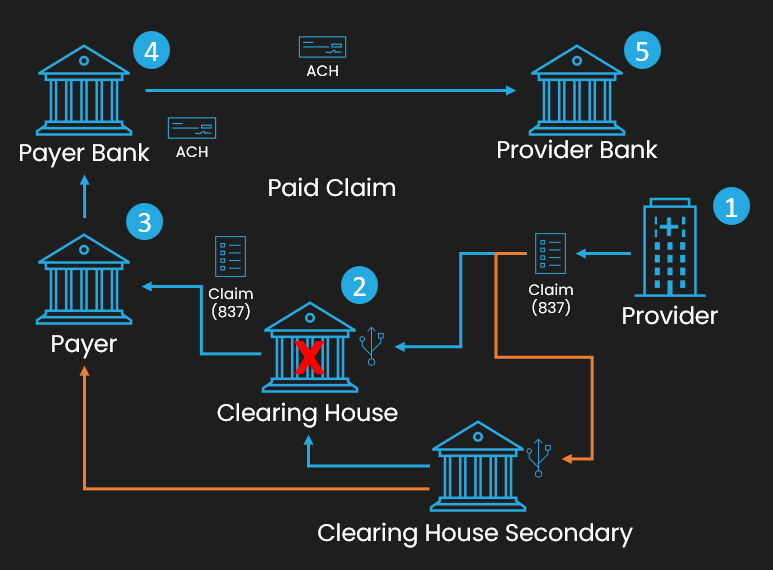
Providers with the ability to use a secondary clearinghouse still can’t get through if the payer doesn’t integrate with that clearinghouse. These exclusive clearinghouse\payer relationships spread the risk of single points of failure throughout the system.
The recent incident with UnitedHealth’s Change Healthcare illustrates the vulnerability of this system. As a dominant clearinghouse that processes claims for a wide array of payers, including Medicaid programs, the cyberattack on its systems led to a complete halt in claim submissions. This disruption had a domino effect, impacting in many cases severely the cash flow of nearly all healthcare providers. As a result, many were compelled to seek emergency funding to continue their operations.
The implications of this design flaw are far-reaching. It raises critical questions about the resilience of our healthcare financial infrastructure and the need for a more robust, diversified system that can better withstand such disruptions. This incident serves as a stark reminder of the need for improved interoperability and reduced reliance on single entities, highlighting the importance of reevaluating and strengthening the structural foundations of our healthcare reimbursement systems.
The Challenges and Benefits of Interoperability in Healthcare
The Promise of interoperability
The concept of interoperability in healthcare is a beacon of hope for transforming patient care and enhancing the efficiency of healthcare systems. At its core, interoperability represents the seamless exchange and utilization of health information across different healthcare platforms and providers. This integrated approach is crucial for enabling healthcare professionals to access and share patient data easily, leading to more informed decision-making and personalized care plans. Such fluid communication not only improves the quality of patient care but also significantly reduces medical errors, contributing to better health outcomes overall.
Another critical aspect of interoperability is its potential to streamline operational processes within the healthcare system. By eliminating redundant tests and reducing administrative burdens, interoperability can lead to considerable cost savings. It simplifies processes like patient data entry, appointment scheduling, and billing, thereby increasing the overall efficiency of healthcare delivery. This efficiency is not just beneficial for healthcare providers but also enhances the patient experience by reducing wait times and improving service quality.
The Current Reality
HL7 FHIR (Fast Healthcare Interoperability Resources) is a standard that has been a catalyst in the quest for interoperability in healthcare. It is designed to simplify and enhance the exchange and interoperability of electronic health records. FHIR combines the best features of HL7’s earlier standards with the latest web technologies, making it both developer-friendly and scalable. This standard supports a wide range of healthcare data formats and workflows, enabling diverse healthcare systems to communicate more effectively. Its flexibility and ease of integration have marked it as a significant advancement in healthcare IT.
In parallel, the X12 standard plays a crucial role in the electronic data interchange (EDI) for administrative and financial transactions in healthcare. It streamlines processes such as billing, claims processing, and information exchange between healthcare providers and payers. X12 helps in reducing paperwork, minimizing errors, and speeding up transaction processing, contributing to the operational efficiency of healthcare organizations.
However, the journey towards achieving true interoperability in healthcare is still in progress. There exists a notable gap between the potential of standards like HL7 FHIR and X12 and their widespread implementation. Healthcare systems often grapple with legacy technologies that are incompatible with newer standards, leading to inconsistent adoption rates and integration challenges. Furthermore, the continuous evolution of these standards necessitates ongoing development and updates, which can be resource-intensive.
The Solutions and Opportunities for Interoperability in Healthcare
The current landscape of healthcare IT is marked by a heavy reliance on external, often opaque software systems. This dependency is more pronounced in healthcare than in many other industries. Integrating Electronic Health Records (EHRs) or Claims systems comes with significant licensing and transaction fees, representing a substantial portion of healthcare organizations’ administrative IT budgets. Unfortunately, these systems are frequently brittle and outdated. The increasing vertical integration seen in clearinghouses exacerbates the issue, creating a scenario where, despite claims of compatibility, there’s an alarming reliance on single points of failure.
The silver lining, however, lies in the burgeoning opportunities for improving interoperability in healthcare. One key solution is the adoption of more open, flexible, and interoperable software systems. By moving away from proprietary, closed systems to those that support dynamic and extensible standards to keep pace with the ever-changing X12 companion guides, healthcare providers can reduce their dependence on single vendors and mitigate the risks associated with single points of failure.
Investment in modernizing legacy systems is another crucial step. Many existing healthcare IT systems are not equipped to handle the complexities of modern healthcare data exchanges. Updating these systems to be more adaptable and capable of integrating with a broader range of platforms can significantly improve interoperability. Many organizations still seek to find a one size fits all solution in an industry that is nearly never the same from provider to provider.
the path to enhanced interoperability in healthcare is multifaceted, involving both technological advancements and cultural changes. By embracing open standards, modernizing legacy systems, leveraging cloud technologies, establishing universal data exchange protocols, and promoting a culture of collaboration, the healthcare industry can move towards a more integrated, efficient, and resilient future.
